Why Do I Have Hallux Valgus?
Overview
 Your big toe is the hardest working toe. Every time your foot pushes off the ground, this toe supports most of your body's weight. Because the big toe is so critical to movement, any problem with it can make walking or even standing painful. A bunion (excess or misaligned bone in the joint) is one of the most common big-toe problems. In addition to causing pain, a bunion changes the shape of your foot, making it harder to find shoes that fit. But you don't have to hobble for the rest of your life. Bunions can be treated. With your doctor's help, your feet can feel and look better.
Your big toe is the hardest working toe. Every time your foot pushes off the ground, this toe supports most of your body's weight. Because the big toe is so critical to movement, any problem with it can make walking or even standing painful. A bunion (excess or misaligned bone in the joint) is one of the most common big-toe problems. In addition to causing pain, a bunion changes the shape of your foot, making it harder to find shoes that fit. But you don't have to hobble for the rest of your life. Bunions can be treated. With your doctor's help, your feet can feel and look better.
Causes
No one single cause has been proven. There are a number of causes, and though shoes can exacerbate the problem, bunions do occur in societies that don?t wear them. We walk on the same type of ground all the time, whereas the human foot was actually designed to adapt to varying terrains. In a sense, a bunion is a type of repetitive strain injury. And like repetitive strain injury, some people are more prone to it than others. One theory, though it remains unproven, is that bunions are caused by one or both of the following. Because the foot wasn?t designed to constantly walk on a level surface, the ball of the big toe is slightly lower than the ball of the rest of your foot. When your foot meets the ground, the ball of the big toe is pushed up, and the big toe joint can?t bend as well as it was designed to. In order for the big toe joint to bend fully as you walk, your foot rolls slightly over to the side (this is also why people with hallux valgus often get hard skin). Also, if your midtarsal joint tends to move from side to side more than it does up and down, the arch in your foot collapses as your foot rolls in. This also makes you more prone to developing bunions. Such problems can be exacerbated by tight footwear. Slip-on shoes can make matters worse. Because they have to be tighter to stay on your feet, you automatically have less room for your toes. And with nothing to hold your foot in place, your toes often slide to the end where they?re exposed to lots of pressure. Likewise, high heels throw more weight onto the ball of the foot, putting your toes under further pressure. If you haven?t got a bunion by adulthood and you later develop one, there could be some underlying arthritis.
Symptoms
In addition to the typical bump, signs of bunions can include red, calloused skin along the foot at the base of the big toe. With bunions, you may also develop calluses on the big toe, sores between the toes, ingrown toenail, and restricted motion of the toe. Some bunions are small and painless and some are large and extremely painful. Pressure from shoes worsens the problem.
Diagnosis
The doctor considers a bunion as a possible diagnosis when noting the symptoms described above. The anatomy of the foot, including joint and foot function, is assessed during the examination. Radiographs (X-ray films) of the foot can be helpful to determine the integrity of the joints of the foot and to screen for underlying conditions, such as arthritis or gout. X-ray films are an excellent method of calculating the alignment of the toes when taken in a standing position.
Non Surgical Treatment
There are two ways to treat this pathological foot conditions, conservatively and surgically. Conservative treatment is the first line treatment which consists of splints and orthotic care to reduce the causative factors. Realigning the foot with the aid of an orthotic helps prevent further degeneration and/or reduce symptoms of HAV in any stage of its deformity. Along with orthotic care, patients may require debridement of corns and calluses produced due to extra forces produced on the foot. Orthotics will also help the function of the big toe joint as it allows it to bend in the correct position. Footwear advice is also essential in the conservative care of bunions, HAV, there may be a need to change footwear, so it is able to fit properly and be compliment with orthotics. Surgical correction of bunions, HAV is available, however should only be considered when conservative care has failed to reduce the onset of bunions, HAV. It is only considered if there is a clear sign that it will induce a better quality of life for the patient. 
Surgical Treatment
When deciding whether to have bunion surgery, there are several things to consider including your age, in children, bunion surgery is often delayed because of the risk of the bunion returning, your medical history and general health, problems with wound healing and infections are more likely in certain conditions such as diabetes, you?re also more likely to develop problems if your bunion is caused by a condition such as rheumatoid arthritis, your occupation and lifestyle, bunion surgery can make your toes less flexible, and you may be unable to return to the same level of physical activity, your expectations of surgery, bunion surgery has about an 85% success rate, but there's no guarantee that your foot will be perfectly straight or pain-free; the success of surgery depends on the type of procedure, the experience of the surgeon and your ability to rest after the operation, the severity of your symptoms, surgery will usually only be recommended if your bunions are causing considerable pain and non-surgical treatments haven't been unsuccessful (because of the associated risks and complications).
What Is Overpronation Of The Feet
To better understand how the muscles and tissue structures in the feet, ankles, legs and hips are adversely affected by overpronation, imagine a person on the end of a bungee cord jumping off a bridge. If the bungee cord gets the right amount of tension on it as the person nears the ground, then he or she will be saved from smashing into the earth. However, if the bungee cord does not pull tight because it is twisted or has no elasticity, then the person will impact the ground with dire consequences. The muscles, tendons, ligaments, and fascia of the legs and feet are the body's bungee cords. If these bungee cords work together, they can protect the joints of the feet and ankles from excessive stress, and prevent muscle and tissue damage caused by overpronation. If they do not work properly, a person will be able to see evidence of this in the feet and ankles, particularly in the alignment of the joints.

Causes
It is important to identify the cause of overpronation in order to determine the best treatment methods to adopt. Not all treatments and preventative measures will work equally well for everyone, and there may be a little trial and error involved to get the best treatment. A trip to a podiatrist or a sports therapist will help you to establish the cause of overpronation, and they will be able to tell you the best treatments based on your specific degree of overpronation and the cause. Overpronation has many causes, with the most common reasons for excessive pronation listed, low arches, flexible flat feet, fallen arches, gait abnormalities, abnormal bone structure, abnormal musculature, bunions, corns and calluses.
Symptoms
Because pronation is a twisting of the foot, all of the muscles and tendons which run from the leg and ankle into the foot will be twisted. In over-pronation, resulting laxity of the soft tissue structures of the foot and loosened joints cause the bones of the feet shift. When this occurs, the muscles which attach to these bones must also shift, or twist, in order to attach to these bones. The strongest and most important muscles that attach to our foot bones come from our lower leg. So, as these muscles course down the leg and across the ankle, they must twist to maintain their proper attachments in the foot. Injuries due to poor biomechanics and twisting of these muscles due to over-pronation include: shin splints, Achilles Tendonitis, generalized tendonitis, fatigue, muscle aches and pains, cramps, ankle sprains, and loss of muscular efficiency (reducing walking and running speed and endurance). Foot problems due to over-pronation include: bunions, heel spurs, plantar fasciitis, fallen and painful arches, hammer toes, and calluses.
Diagnosis
Bunions, calluses and crooked toes may indicate alignment problems. So, it is important to ascertain the condition of a client's toes. Check the big toe to determine if the first joint of the toe is swollen, has a callus or bunion, and/or looks as though it abducts (i.e., hallux valgus) rather than pointing straight ahead. Also, look to see if the lesser toes seem to "curl up" (i.e., the person has hammer or claw toes). This may be indicative of damage to, or inflexibility of the plantar fascia caused by excessive flattening of the foot.

Non Surgical Treatment
The following exercises help retrain the foot and ankle complex to correct overpronation. Exercises may be performed while wearing shoes, or for an even greater challenge, in bare feet. Duck Stand. This exercise is designed to prepare for the more dynamic BT exercises ahead by waking up the gluteal muscles and teaching clients how the gluteal muscles control the degree of foot pronation. For example, when the glutes contract concentrically, they rotate the leg outward. As the leg rotates outward, the arch of the foot raises (i.e., supinates). Stand beside the BT with both heels together and feet turned outward. (Note: As you progress, perform this exercise while standing on the BT.) Try to rotate legs outward by tightening buttock muscles while tilting pelvis under. As legs rotate outward, arches of the feet raise up out of pronation. Hold position for 30 seconds. Big Toe Pushdowns. This exercise is designed to strengthen the muscle of the big toe that holds up the arch of the foot (i.e., flexor hallucis longus muscle). This stops the foot from overpronating. Stand on top of the BT dome with feet facing forward. Use gluteal muscles to raise the arches of the feet (see previous exercise - "Duck Stand"). Keep arches raised while pushing down big toe into the BT. While pushing down, tension build in the arch on the underside of their foot should be felt. Hold position for 15 seconds.
Prevention
Pronation forces us to bear most of our weight on the inner border of our feet. Custom-made orthotics gently redistributes the weight so that the entire foot bears its normal share of weight with each step we take. The foot will not twist out at the ankle, but will strike the ground normally when the orthotics is used. This action of the custom-made orthotics will help to prevent shin splints, ankle sprains, knee and hip pain, lower back pain, nerve entrapments, tendonitis, muscle aches, bunions, generalized fatigue, hammer toes, and calluses.
Severs Disease Physical Rehabilitation
Sever?s disease occurs in children when the growing part of the heel is injured. This growing part is called the growth plate. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become ?tight.? The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This may injure the heel.
Causes
The condition generally occurs in active children at early adolescence during rapid growth periods as the heel bone can grow faster than the leg muscles causing them to become tight and overstretched. Sever?s disease most often caused by inadequate footwear, playing sport on hard surfaces, calf tightness and biomechanical problems.
Symptoms
Severs causes swelling, pain and tenderness over the back of the heel. Your child may walk with a limp. Initially the pain may be intermittent occurring only during or after exercise. As the problem gets worse, pain may be present most of the time. The swelling increases and is painful when touched or knocked. It commonly affects boys who are having a growth spurt during their pre-teen or teenage years. One or both knees may be affected.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
It is important that those with Sever?s Disease are treated by a medical professional to reduce pain and allow children to continue to participate in sporting activities. The Athlete?s Foot recommends a visit to your local medical professional to be diagnosed correctly and receive specialised care. Symptoms include pain through the back of the heel where the Achilles tendon inserts into the heel bone, pain during activity especially running and jumping and the back of the heel may be tender to touch.
Achilles Tendon Operation Recovery Time
Overview
 An Achilles tendon injury can affect both professional and amateur athletes. The Achilles tendon is one of the longer tendons in your body, stretching from the bones of your heel to your calf muscles. You can feel it, a springy band of tissue at the back of your ankle and above your heel. It allows you to extend your foot and point your toes to the floor. Unfortunately, it's a commonly injured tendon. Many Achilles tendon injuries are caused by tendinitis, in which the tendon becomes swollen and painful. In a severe Achilles tendon injury, too much force on the tendon can cause it to tear partially or rupture completely.
An Achilles tendon injury can affect both professional and amateur athletes. The Achilles tendon is one of the longer tendons in your body, stretching from the bones of your heel to your calf muscles. You can feel it, a springy band of tissue at the back of your ankle and above your heel. It allows you to extend your foot and point your toes to the floor. Unfortunately, it's a commonly injured tendon. Many Achilles tendon injuries are caused by tendinitis, in which the tendon becomes swollen and painful. In a severe Achilles tendon injury, too much force on the tendon can cause it to tear partially or rupture completely.
Causes
Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2.5 inches (6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, falling from a height, stepping into a hole.
Symptoms
Patients with an Achilles tendon rupture will often complain of a sudden snap in the back of the leg. The pain is often intense. With a complete rupture, the individual will only be ambulate with a limp. Most people will not be able to climb stairs, run, or stand on their toes. Swelling around the calf may occur. Patients may often have had a sudden increase in exercise or intensity of activity. Some patients may have had recent corticosteroid injections or use of fluoroquinolone antibiotics. Some athletes may have had a prior injury to the tendon.
Diagnosis
Some patients mistakenly believe the tendon is working if they can push the foot down, however, patients will usually be able to move the foot up and down while sitting because the other surrounding muscles and tendons are still intact. Trying to push up while standing and applying body weight to the foot will reveal the true weakness. Sensation and circulation to the foot and ankle will be normal. In addition, x-rays will be normal unless the Achilles injury involves pulling off (avulsion) of the bone on the calcaneus (heel bone). This is quite rare, occurring in only a small fraction of patients with Achilles injuries. Patients suffering this type of Achilles avulsion injury tend to be older with weaker bone. Imaging Studies. Plain x-rays will be negative in patients who have suffered an Achilles tendon rupture. The rupture can be seen on ultrasound or MRI. However, these studies are not indicated for acute ruptures unless there is some uncertainty about the diagnosis. For chronic problems of the Achilles or ruptures that are old, an MRI may be very helpful.
Non Surgical Treatment
A medical professional will take MRI scans to confirm the diagnosis and indicate the extent of the injury. Sometimes the leg is put in a cast and allowed to heal without surgery. This is generally not the preferred method, particularly for young active people. Surgery is the most common treatment for an achilles tendon rupture. 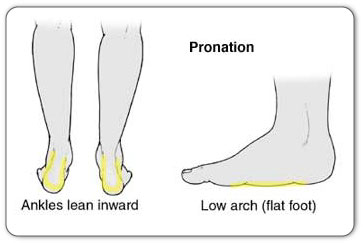
Surgical Treatment
Surgery could allow for a quicker healing time. The procedure generally involves making an incision in the back of your lower leg and stitching the torn tendon together. Depending on the condition of the tissue, the repair may be reinforced with other tendons. As with any surgery, the main complication is the risk for infection, however, this risk is reduced by using smaller incisions.
Prevention
You can help to reduce your risk of an injury to your Achilles tendon by doing the following. When you start a new exercise regime, gradually increase the intensity and the length of time you spend being active. Warm up your muscles before you exercise and cool them down after you have finished. The benefit of stretching before or after exercise is unproven. However, it may help to stretch your calf muscles, which will help to lengthen your Achilles tendon, before you exercise. Wear appropriate and well-fitting shoes when you exercise.
True Leg Length Discrepancy Test
Limb-length discrepancies or differences are conditions that result in limbs that are unequal in length or that exhibit other anomalies. The conditions occur when bones or joints in the arms or legs are abnormal or become damaged. Providers might refer to these conditions as limb-length discrepancies, limb differences or limb-length conditions.

Causes
Common causes include bone infection, bone diseases, previous injuries, or broken bones. Other causes may include birth defects, arthritis where there is a loss of articular surface, or neurological conditions.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
The evaluation of leg length discrepancy typically involves sequential x-rays to measure the exact discrepancy, while following its progression. In addition, an x-ray of the wrist allows us to more carefully age your child. Skeletal age and chronological age do not necessarily equal each other and frequently a child's bone age will be significantly different than his or her stated age. Your child's physician can establish a treatment plan once all the facts are known: the bone age, the exact amount of discrepancy, and the cause, if it can be identified.
Non Surgical Treatment
Heel lifts and sole lifts are simple ways Pedorthists can compensate for leg length deficiencies. These small modifications can make a tremendous difference to a person?s comfort, balance and mobility. Although people do not always know if they have LLD if you have any of the symptoms I have mentioned you should consult a Pedorthist as treating your condition early will reduce the development of serious problems later on.

Surgical Treatment
Surgery is another option. In some cases the longer extremity can be shortened, but a major shortening may weaken the muscles of the extremity. In growing children, lower extremities can also be equalized by a surgical procedure that stops the growth at one or two sites of the longer extremity, while leaving the remaining growth undisturbed. Your physician can tell you how much equalization can be attained by surgically halting one or more growth centers. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the LLD will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical; the goal is to attain equal length of the extremities at skeletal maturity, usually in the mid- to late teens. Disadvantages of this option include the possibility of slight over-correction or under-correction of the LLD and the patient?s adult height will be less than if the shorter extremity had been lengthened. Correction of significant LLDs by this method may make a patient?s body look slightly disproportionate because of the shorter legs.
Treatment Of Flat Feet In Adults
Overview
Adult flatfoot refers to a deformity that develops after skeletal maturity is reached. Adult flatfoot should be differentiated from constitutional flatfoot, which is a common congenital non-pathologic foot morphology. There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. 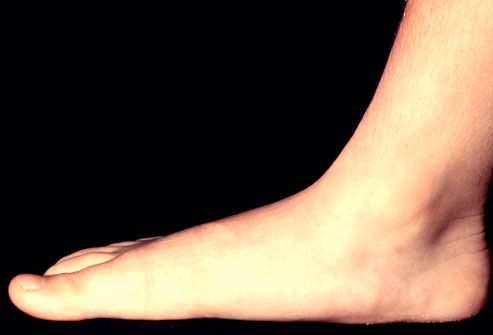
Causes
Adult acquired flatfoot is caused by inflammation and progressive weakening of the major tendon that it is responsible for supporting the arch of the foot. This condition will commonly be accompanied by swelling and pain on the inner portion of the foot and ankle. Adult acquired flatfoot is more common in women and overweight individuals. It can also be seen after an injury to the foot and ankle. If left untreated the problem may result in a vicious cycle, as the foot becomes flatter the tendon supporting the arch structure becomes weaker and more and more stretched out. As the tendon becomes weaker, the foot structure becomes progressively flatter. Early detection and treatment is key, as this condition can lead to chronic swelling and pain.
Symptoms
Often, this condition is only present in one foot, but it can affect both. Adult acquired flatfoot symptoms vary, but can swelling of the foot's inner side and aching heel and arch pain. Some patients experience no pain, but others may experience severe pain. Symptoms may increase during long periods of standing, resulting in fatigue. Symptoms may change over time as the condition worsens. The pain may move to the foot's outer side, and some patients may develop arthritis in the ankle and foot.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise. A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet - the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non surgical Treatment
Although AAF is not reversible without surgery, appropriate treatment should address the patient?s current symptoms, attempt to reduce pain, and allow continued ambulation. In the early stages, orthotic and pedorthic solutions can address the loss of integrity of the foot?s support structures, potentially inhibiting further destruction.3-5 As a general principle, orthotic devices should only block or limit painful or destructive motion without reducing or restricting normal motion or muscle function. Consequently, the treatment must match the stage of the deformity. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
Tibial Posterior Tendon Dysfunction Symptoms
Overview
A variety of foot problems can lead to adult acquired flatfoot deformity (AAFD), a condition that results in a fallen arch with the foot pointed outward. Most people - no matter what the cause of their flatfoot - can be helped with orthotics and braces. In patients who have tried orthotics and braces without any relief, surgery can be a very effective way to help with the pain and deformity. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided. 
Causes
There are a number of theories as to why the tendon becomes inflamed and stops working. It may be related to the poor blood supply within the tendon. Increasing age, inflammatory arthritis, diabetes and obesity have been found to be causes.
Symptoms
PTTD begins with a gradual stretching and loss of strength of the posterior tibial tendon which is the most important tendon supporting the arch of the human foot. Left untreated, this tendon will continue to lengthen and eventually rupture, leading to a progressive visible collapse of the arch of the foot. In the early stages, patients with PTTD will notice a pain and swelling along the inner ankle and arch. Many times, they are diagnosed with ?tendonitis? of the inner ankle. If the foot and ankle are not properly supported during this early phase, the posterior tibial tendon can rupture and devastating consequences will occur to the foot and ankle structure. The progressive adult acquired flatfoot deformity will cause the heel to roll inward in a ?valgus? or pronated direction while the forefoot will rotate outward causing a ?duckfooted? walking pattern. Eventually, significant arthritis can occur in the joints of the foot, the ankle and even the knee. Early diagnosis and treatment is critical so if you have noticed that one, or both, of your feet has become flatter in recent times come in and have it checked out.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Treatment depends very much upon a patient?s symptoms, functional goals, degree and specifics of deformity, and the presence of arthritis. Some patients get better without surgery. Rest and immobilization, orthotics, braces and physical therapy all may be appropriate. With early-stage disease that involves pain along the tendon, immobilization with a boot for a period of time can relieve stress on the tendon and reduce the inflammation and pain. Once these symptoms have resolved, patients are often transitioned into an orthotic that supports the inside aspect of the hindfoot. For patients with more significant deformity, a larger ankle brace may be necessary. 
Surgical Treatment
For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.